Dysphagia Assessment: Have You Considered the Esophagus?
December 28, 2023
4 min. read

To perform an accurate dysphagia assessment, we must understand the interrelationship between all stages of swallowing—the oral, pharyngeal, and esophageal phases. Each stage plays a unique role, and issues in one can affect others, especially when symptoms suggest an esophageal concern.
While speech-language pathologists don't diagnose esophageal disorders, they must recognize when to refer patients to a gastroenterologist for further testing. This knowledge is essential to ensure that patients receive proper care and the support they need to address their dysphagic complaints.
In this article, we will explore how an accurate esophageal dysphagia assessment can help you identify potential issues and provide guidance on when further evaluation might be necessary.
Recognizing hidden causes in dysphagia
Symptoms of esophageal dysphagia can vary widely, from a sensation of food sticking in the throat to subtle signs that may suggest a referral is needed. Patients may report intermittent chest discomfort, difficulty swallowing both solids and liquids, or even regurgitation—all of which can indicate an esophageal origin. However, it is easy to overlook an esophageal cause when the patient's complaint appears focused in the oral or pharyngeal regions.
Patients often assume that where they feel discomfort is where the issue originates, but the esophagus may be the true source. This misperception highlights the importance of considering esophageal factors during a dysphagia assessment.
For instance, patients may localize their complaints to the neck when the primary disorder is in the esophagus. Those with distal narrowing of the esophagus often point to the pharyngeal region, indicating where they sense an obstruction. Similarly, patients with esophageal achalasia may refer their symptoms to the neck, underscoring the need for a holistic approach in evaluating dysphagia.
As SLPs, we must remember that the stages of swallowing—oral, pharyngeal, and esophageal—are interdependent. Events in one stage can impact the others, particularly with primary esophageal dysphagia, which frequently affects both upstream oral and pharyngeal functions. Recognizing these interdependencies allows for a more comprehensive assessment and supports better patient outcomes.
Structural and functional issues in esophageal dysphagia
In an esophageal dysphagia assessment, its essential to consider both structural and functional issues in the esophagus that can complicate swallowing across stages. The following examples illustrate how these distinct types of esophageal disorders can affect the entire swallowing process, even when symptoms are not localized to the esophagus itself.
Obstructed esophagus
An obstructed esophagus is a common example of a structural issue that can significantly impact swallowing. When a blockage prevents food from passing smoothly, it can lead to a backup effect, where patients struggle to clear food at the pharyngeal stage.
In cases like this, an esophageal dysphagia assessment that includes imaging can reveal the root cause of the obstruction and prevent misinterpretation of symptoms as solely oral or pharyngeal issues.
Scleroderma
On the other hand, scleroderma exemplifies a systemic and motility-related disorder that impacts esophageal function. By disrupting the smooth muscle function of the esophagus, scleroderma can indirectly affect pharyngeal function, as patients often experience difficulties initiating swallows due to inefficient esophageal peristalsis.
This example highlights why esophageal dysphagia assessment should include awareness of both motility issues and systemic conditions, as they can affect swallowing beyond the esophagus.
An insightful approach to esophageal dysphagia assessment
A comprehensive esophageal dysphagia assessment goes beyond surface symptoms to address potential underlying issues within the esophageal stage. By focusing on both structural and functional factors, you can determine if esophageal dysfunction contributes to the patients swallowing difficulties. This type of assessment typically includes:
Patient history: Collect a thorough history of symptoms, including duration, onset, and location of discomfort. Detailed symptom reports can help clinicians recognize esophageal indicators that may initially seem unrelated to swallowing.
Imaging: Use imaging tools, such as a barium swallow study or endoscopy, to visualize the esophagus and identify abnormalities like strictures, blockages, or motility issues that might impact the swallowing process.
Referral pathways: Recognize when specialized input from gastroenterology is warranted. Esophageal dysphagia often requires a collaborative approach, especially if symptoms point to complex structural or systemic conditions beyond the SLP's scope.
By conducting a thorough esophageal dysphagia assessment, you gain valuable insights into the root causes of symptoms, allowing for more accurate diagnoses and targeted referrals that support comprehensive patient care.
Supporting better patient outcomes in dysphagia care
As speech-language pathologists specializing in dysphagia, we must maintain a working knowledge of esophageal disorders and the ways in which different swallowing stages interact. Patients rely on our comprehensive, accurate assessments and timely referrals when necessary.
Performing a thorough esophageal dysphagia assessment involves not only visualizing the esophageal phase of swallowing but also taking a detailed patient history to identify possible esophageal involvement. This holistic approach is key to supporting patient outcomes and ensuring that all underlying causes are addressed.
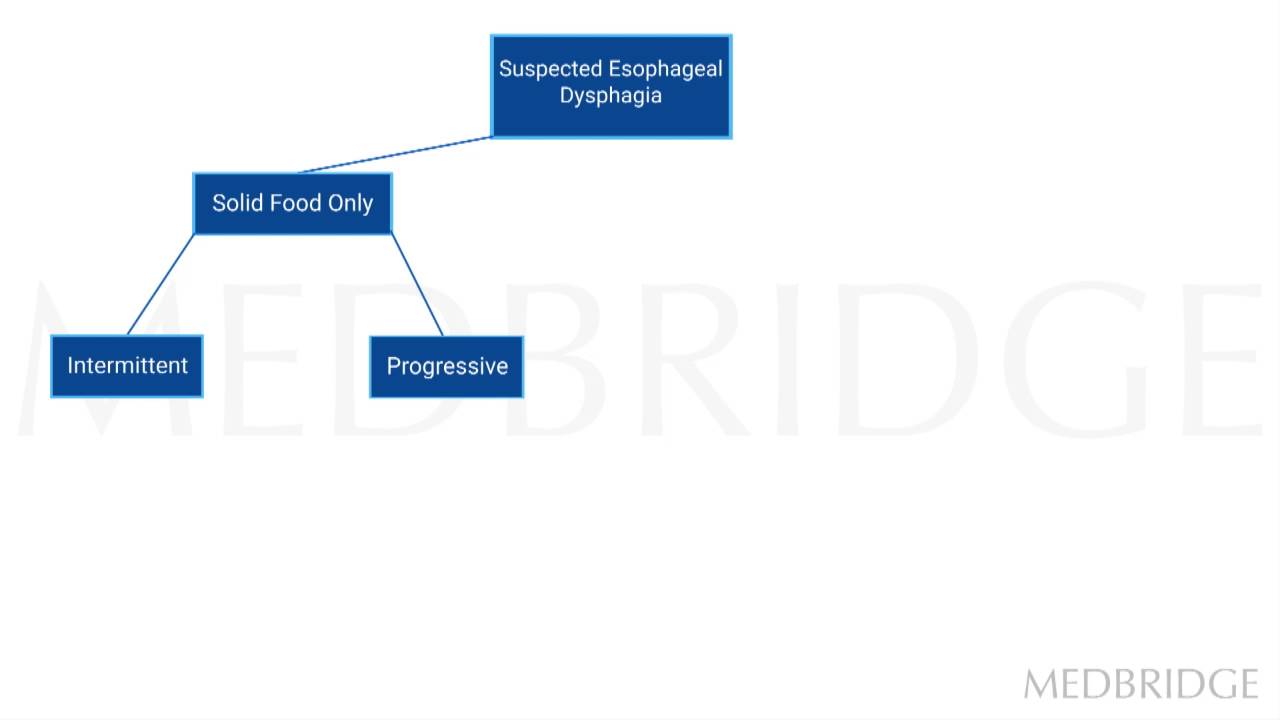
Below, watch a short video from Dr. Michael Groher’s course, Disorders of the Esophagus for the Speech-Language Pathologist, as he discusses the Esophageal Disorder Decision Tree.