Female Athlete Triad: Five Key Takeaways
Female athletes are participating in sports at record levels. Anatomic and physiological differences exist between female and male athletes including the Female Athlete Triad. The sports medicine team should consider both the short- and long-term effects of the triad when treating female athletes of all ages and abilities.
Meet Susan
Susan is a 15-year old high-school cross-country and track athlete, who is a “running prodigy” having won several national events while in junior high school. She is part of a high-level local running development club and is mentored by a former Olympic runner. She trains 50 weeks out of the year, and is a top prospect for several Division 1 colleges.
Susan has struggled with shin pain each season throughout her high school career, but during her sophomore year she has been sidelined from competition and all road races due to a stress fracture of the right tibia. Her scholarship hopes are on the line…
What is the Female Athlete Triad?
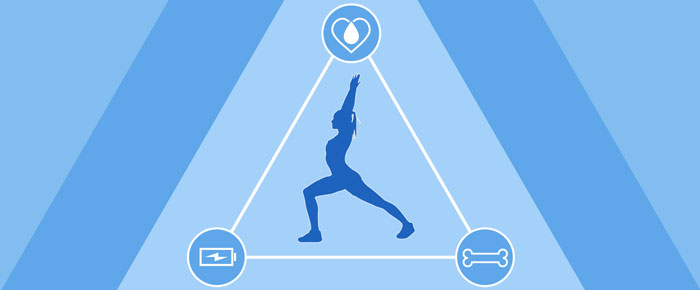
The female athlete triad is the relationship originally observed between three related clinical conditions: eating disorders, menstrual irregularities, and bone health. This concept has evolved since its initial description in 1992 and now includes the spectrum between optimal and non-optimal states of these components. Often, the female athlete moves along these spectra throughout her lifetime and competitive history.3
The three components of the triad are highly interrelated, and are believed to be strongly linked to energy availability – the “lynchpin” of the Triad. The triad may be related to long-term pathology, including permanent loss of bone mineral density.
For example, our athlete Susan may have moved from a state of “optimal bone health” to a state of “low bone mineral density,” leading to the stress fracture in her right tibia. But why did this happen? Is it solely due to her demands of sport and progression over time? Is it optimal for Susan to continue to train as she has been?
Without further information, it is not possible to know whether her menstrual or nutritional status (energy availability) have contributed. In many women with the triad, purposive or inadvertent low energy availability negatively affects both menstrual status and bone health. A multidisciplinary approach to evaluation and treatment should be used with athletes who may have facets of the triad.2
Many women have no idea that cessation of menstruation is a warning sign! Athletes like Susan must be examined and screened by a physical therapist for the components of the triad. Then, any existing dysfunctions can be addressed appropriately. Simply treating her stress fracture or assessing her musculoskeletal system is not enough!
Five Key Takeaways
1. The triad is often denied, unrecognized, or under-reported
All sports medicine personnel should learn to recognize and prevent it. As vital members of the sports medicine team, physical therapists and athletic trainers should have working knowledge of the facets of the triad.
2. Be ready to evaluate for risk of the triad
Don’t be leery of asking the right questions that deal with menstruation and eating and eating disorders.
- During the examination, seek the athlete’s menstrual history and current function with simple questions: “How old were you when you began to menstruate?” and “Do you have a monthly period?”
- Ask questions about their nutrition and diet or screen for an eating disorder.1 The Triad Consensus Panel recommends asking the following screening questions at the time of the sport pre-participation evaluation.
- Note: With minors, have the parent present.
| Triad Consensus Panel Screening Questions2 |
|---|
|
3. Refer to the appropriate medical or allied health provider if even ONE component of the triad is present
You will need to develop referral strategies with professionals qualified to evaluate and treat athletes with the triad, including:
- Family medicine or internal medicine physician
- Endocrinologist
- Sports psychologist
- Registered dietician (with expertise in sports nutrition)
Don’t be alarmist, but don’t hesitate!
4. Educate coaches and parents about the triad
Avoid pressuring athletes! Deconstruct weight and performance myths such as “the less you weigh the better you will perform.” A better-informed community can help with prevention.
5. Educate athletes about the warning signs and risks of the triad
Offer a “recipe for success” in athletics and physical performance, including healthy training strategies, optimal nutritional support, rest, and varied activities (avoidance of specialization). You can use this publicly available document for Education of Parents, Athletes, and Coaches from the Female Athlete Triad Coalition.
Best care of the female athlete includes knowledge, assessment, and readiness to treat the female athlete triad. Every physical therapist and athletic trainer should know the three components of the triad and have referrals for managing the aspects beyond our scope of practice. Finally, educate your peers, your communities, and female athletes from all walks of life.
- Cotton M, Ball C, Robinson P. Four Simple Questions can help screen for eating disorders. J Gen Intern Med. 2003;18:53-56.
- DeSouza MJ, Nattiv A, Joy E, Misra M, Williams NI, Mallinson RJ, Gibbs JC, Olmstead M, Goolsby M, Matheson G, Expert Panel. The 2014 Female Athlete Triad Coalition Consensus Statement on Treatment and Return to Play of The Female Athlete Triad: 1st International Conference held in San Francisco CA, and 2nd International Conference held in Indianapolis, IN. British Journal of Sports Medicine, 2014;48:289-309.
- Nattiv A, Loucks AB, Manore MM, Sanborn CF, Sundgot-Borgen J, Warren MP. American College of Sports Medicine Position Stand: The Female Athlete Triad. Medicine & Science in Sports & Exercise. 2007;1867-1882.

