Are Special Tests Necessary? Why You Should Also Use Symptom Modification Procedures
April 12, 2018
4 min. read

Weare always looking to provide the best, most specific treatment for our patients. With both special tests and symptom modification procedures in your toolbox, you can educate your patients on what anatomical structures are impacted, why these structures are irritated, and how to best address the underlying cause of the dysfunction.
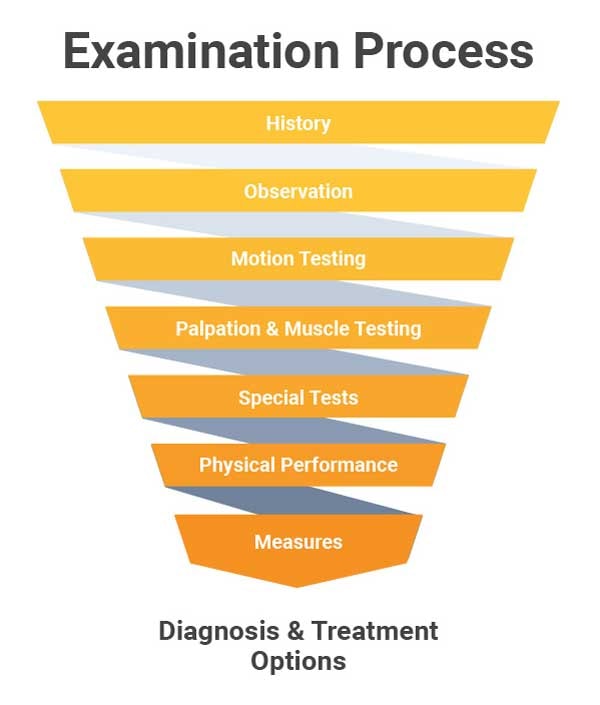
The Place of Special Tests in the Exam Process
The examination process includes many steps that ultimately result in providing you with a diagnosis and appropriate treatment options. Using special tests with good sensitivity, specificity, and likelihood ratios provide quality data to confirm and/or refute your diagnostic hypotheses. Good data from these tests allow you to determine appropriate treatment options and provide correct prognostic information to your patient.1
Research has been guiding us, as a profession, toward specific special tests and clusters of tests which provide us with greater diagnostic accuracy.2 For example in the Medbridge course, Evidence-based Examination of the Shoulder, Eric Hegedus, PT, DPT, MHSc, OCS, CSCS,provides up to date research on the best special tests for the shoulder and also indicates that future research may yield even better test clusters.
After youperform your examination andhone in on the appropriate diagnosis, you may find yourself asking, what next?. Have you identified the impairment with the greatest impact on your patients symptoms?
Use of Symptom Modification Procedures (SMPs)
An SMP is the application of an outside force which changes a movement pattern or muscle activation pattern in order to reduce the severity of a patients symptoms with a particular activity. Even with asymptomatic movements, application of an SMP can improve the quality of a motion or the overall range of motion. This can be applied early on in the motion testing portion of the examination process.
3 Benefits of Using SMPs Early in the Exam
Improve patient buy-in- Since you have diminished the patients symptoms quickly, the patient will have confidence that you are on the right track and are capable of helping.
Simplify your objective examination- Now that you have effectively identified the specific movement pattern contributing to the patients symptoms, you can focus on the specific mobility, muscle performance, or motor control deficits that contribute to the faulty movement pattern.
Choose effective intervention -Identifying the faulty movement pattern and underlying factors contributing to this pattern can lead you to interventions specific to correcting these contributing factors.
Combining SMPs & Special Test Clusters in Practice
Here are two examples of SMPs with shoulder active motion testing to treat subacromial impingement with subacromial bursitis:3
Glenohumeral fault
If the patient demonstrates excessive humeral internal rotation during active shoulder flexion, the therapist can manually externally rotate the humeral head in order to increase the subacromial space and assess the impact on the patients symptoms. The author has provided the video below as an example:
[iframe id="https://www.youtube.com/embed/-0fsAiI3_lM" align="center" thumbnail="https://img.youtube.com/vi/-0fsAiI3_lM/maxresdefault.jpg"]
Scapulothoracic fault
One special test that doubles as an SMP is the scapular assist test which increases the upward rotation of the scapula during active shoulder flexion. Since this test is positive when it reduces the patients symptoms, it guides you toward interventions to improve scapular upward rotation. A positive test also guides the therapist to assess for scapulothoracic pseudo-joint mobility deficits and muscle performance deficits of the scapular upward rotators. The author has provided the video below as an example:
[iframe id="https://www.youtube.com/embed/-IDhWZ-l35w" align="center" thumbnail="https://img.youtube.com/vi/-IDhWZ-l35w/maxresdefault.jpg"]
Now that you have identified impairments contributing to the patients symptoms, make sure to use a special test cluster to adequately identify the patients diagnosis. In this case a systematic review by Hegedus et al recommends combing Hawkins-Kennedy, Neer, Painful Arc, Empty Can, and Resisted ER for subacromial impingement. With three or more positive special tests, you are ready to educate the patient on your findings.
Expanding Your Toolbox
Special tests and SMPs in combination can provide us with a means to provide the best, most specific treatment for our patients. Here are three key reasons to bring this dynamic duo into your practice:
Special tests provide us with diagnostic information to identify the particular tissues involved, while SMPs help indicate the movement patterns contributing to the patients symptoms and where we should target our interventions.
Both special tests and SMPs can aid in educating your patient on what anatomical structures are impacted, why these structures are being irritated, and how to best address the underlying cause of the dysfunction.
SMPs can make an immediate impact, try adding them into your evaluations to WOW your patient in the first 5 minutes of your objective exam!
Below, watch one of the MedBridge Patient Education videos on Shoulder Impingement: