4 Tips for Conducting Successful E-Visits

Like many of you, I’m trying to navigate the current COVID-19 crisis. My goal is to keep my patients safe while also delivering modified, quality service. E-visits are one option for staying connected with your patients while still providing them with advice so they can continue progressing.
An e-visit is defined as non-face-to-face, patient-initiated communication with a health care provider. Current legislative and reimbursement issues are real barriers to telehealth, so e-visits are a plausible, short-term stopgap solution while the industry works toward full telehealth implementation.
1. E-Visits Must Be Patient-Initiated
An e-visit must be initiated/requested by the patient with their consent and be reflected in your documentation. Therefore, scheduling the visit may be beneficial vs. calling down a list of patients.
Successful reimbursement for e-visits is outside the scope of this specific article, but making sure that e-visits are patient initiated is one necessary step in order to ensure reimbursement. For more information on this topic, refer to MedBridge’s recent webinar, “Updates on E-Visits and Telehealth for Outpatient Therapy Services, Part 1,” as well as the blog post, “FAQ: Providing E-Visits During the COVID-19 Crisis.”
 2. Refer to the Chart and Home Exercise Program
2. Refer to the Chart and Home Exercise Program
Don’t be tempted to speak to your patient utilizing only your memory. Treat the e-visit like you would a regular face-to-face visit. Utilize documentation to improve your recall of prior assessments and home exercise programs (HEP).
Statements like, “I’m comparing your initial assessment to what you’re telling me today,” add value to your visit by indicating you care about their progress. Documentation review also allows for clarification statements like, “You’re reporting the pain has spread to the lower part of your leg when, initially, we discussed that it was isolated to the upper part of the hip. Is that accurate?”
These types of insights allow you to maximize clinical reasoning even at a distance.
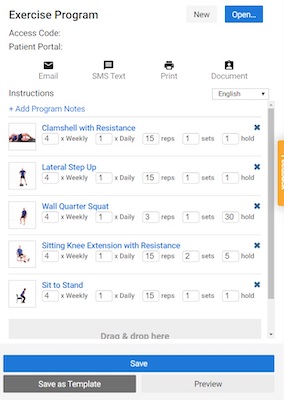
Access the most recent version of the assigned HEP and encourage your client to do the same. This way, you both can reference the HEP, which helps to increase clarity in a verbal-only discussion.
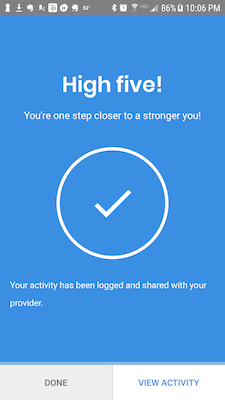 Encourage your patient to utilize technology that supports adherence to the HEP. Adherence tends to be better with a remote HEP application versus a paper-only handout anyway.1 As an example, the MedBridge GO app offers reminders to patients to complete their HEP and also provides positive feedback upon completion.
Encourage your patient to utilize technology that supports adherence to the HEP. Adherence tends to be better with a remote HEP application versus a paper-only handout anyway.1 As an example, the MedBridge GO app offers reminders to patients to complete their HEP and also provides positive feedback upon completion.
3. The Subjective Interview Is Key
Conducting a thorough interview and actively listening to your patients’ concerns and goals is key during any therapy visit, and that importance is only heightened with an e-visit.
The subjective interview is often more powerful than most clinicians realize. Therapists tend to focus on physical examination methods like special testing, range of motion, and strength testing. But when compared to an MRI, subjective history diagnosis agreed 75% of the time.2 For follow-up treatments, subjective information can give clinicians enough data to make informed decisions about exercise progression, activity modification, and grade return to normal prior level of function.
During your e-visit subjective interview, ask about how the patient has been feeling since their last visit along with how they feel the exercise program has been going. Other strategies you can use include:
- While referencing to your patient’s current home program, ask about the difficulty of specific exercises.
- Use a rated perceived exertion scale. This powerful tool allows you to accurately change and or dose exercise remotely.
- Discuss the severity, nature, and quality of any pain your patient is having in order to get a sense for current irritability levels so you can make informed decisions about interventions.
- Ask about observations you would normally make in the clinic. For example:
- Are you walking normally or with a limp?
- Can you walk in a straight line?
- Are you able to put all of your weight through your affected lower extremity?
- Have you had any changes in breathing?
- Have you noticed any skin or wound changes? Has there been drainage?
4. Practice Active Listening
Actively listening allows you to meet your patients’ goals even by phone and will guide changes in intervention during an e-visit. Shared decision making is still a primary goal in this context.
When you’re wrapping up a call, try asking, “What else can I do for you today?” as opposed to “Do you have any other questions?” This subtle difference can lead to more engagement at this point in the e-visit and indicates you’re not in a rush to end the interaction.
Following these e-visit strategies will help you maximize clinical reasoning and patient outcomes. Many of these concepts will translate well when you are able to transition to full telehealth visits.
Disclaimer: The information in this blog post (“Post”) is provided for general informational purposes only, and may not reflect the current law in your jurisdiction. No information contained in this Post should be construed as legal advice from MedBridge, Inc., or the individual author, nor is it intended to be a substitute for legal counsel on any subject matter.
- Lambert, T. E., Harvey, L. A., Avdalis, C., Chen, L. W., Jeyalingam, S., & Pratt, C. A., et al. (2017). An app with remote support achieves better adherence to home exercise programs than paper handouts in people with musculoskeletal conditions: a randomised trial. Journal of Physiotherapy, 63(3): 161–167.
- Somerville, L. E., Willits, K., Johnson, A. M., Litchfield, R., LeBel, M.-E., & Moro, J., et al. (2017). Diagnostic validity of patient-reported history for shoulder pathology. Surgery Journal (New York, N.Y.), 3(2): e79–e87.

