More Than Just Footrests: Positioning the Lower Extremities
September 29, 2020
9 min. read

Carol, a patient of yours who uses a wheelchair, has just arrived for her regular appointment. Upon first seeing her, you can tell immediately that her lower extremities are not properly aligned. In fact, one foot is off the footrest and dragging slightly; plus, during your assessment, she comments that shes been having pain in her hips and feels like she might be at risk of sliding out of the chair.
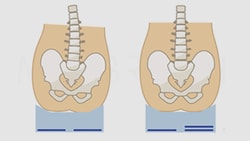
While her concerns appear to be related to her legs, the positioning of the lower extremities is highly dependent on the positioning of the pelvis. Its also important that the lower extremities bear weightif possibleto distribute pressure along the posterior thighs and under the feet to help increase stability.
What should you be checking for to help keep Carols lower extremities aligned, reduce the risk of injury, and improve her comfort?
Hip Flexion
What Is It?
Some patients dynamically pull their hips into flexion. Others may have lost range of motion and, as a result, the hip cannot be extended to a reasonable position for sitting.
What Causes It?
Loss of ROM may occur due to poor ROM management or poor positioning, although some patients dynamically flex the hip in an attempt to stabilize or hang on.
How Should I Solve It?
If the hip flexion is flexible or dynamic, you can provide strapping over the feet. If the hip flexion is fixed, the seat-to-back angle must be closed to match the upper-leg-to-trunk angle. This is often done by placing a wedge under the seat itself. Pulling the thigh downward into extension will only pull the pelvis into an anterior tilt.
What Is the Goal?
In a flexible scenario, goals include providing stability and keeping the feet on the footplates to prevent injury and promote weight bearing. In a fixed scenario, the goal is to prevent anterior pelvic tilt.
Hip Extension
What Is It?
Hip extension is a flexible or fixed extended posture of the hip.
What Causes It?
Some patients dynamically extend at the hip, often as a part of a total extensor pattern. Other patients may have lost ROM and the hip cannot be flexed to a 90-degree angle. Although many patients are positioned at a greater than 90-degree seat-to-back angle, 90 degrees of hip flexion is generally required for a seated position. Some patients who actively extend are attempting to unweight a painful hip.
How Should I Solve It?
If the hip extension is dynamic, strategies can be employed to reduce overall extension. If there is a range limitation, the seat-to-back angle needs to be opened to accommodate this.
Although you may be able to flex the upper leg, if hip flexion is limited, you will only push the pelvis back into a posterior pelvic tilt. If the hamstrings are tight, increasing knee flexion may also be helpful.
Occasionally, a patient will have more hip flexion available on one side of their body than the other. In this case, a specialized seat can be used (either off the shelf or molded) to allow for the limitation in hip flexion on one side while taking advantage of a functional range on the other side. By flexing one side where range is available (generally to 90 degrees), you can prevent further loss of hip flexion range on this side while making it easier to keep the patient back on their seat. When a patient is positioned in hip extension, it is hard to keep the pelvis back in the seat.
What Is the Goal?
The goals of addressing hip extension in the seating system include preventing further ROM losses, which could lead to a more reclined and less functional position, affecting vision, feeding, and respiratory function.
Hip Adduction
What Is It?
Hip adduction causes the legs to come together at midline.
What Causes It?
Hip adduction is often a component of extension and can also result from loss of range.
How Should I Solve It?
Many off-the-shelf cushions include a generic contour to encourage the upper legs to align with the hips. If this is not adequate to limit adduction, a medial knee support or block, sometimes called a pommel, is often used.
It should be noted that some folks have used medial knee blocks inappropriately in an attempt to keep the pelvis back in the seating system. The purpose of this seating component is to keep the legs in alignment with the hips, limiting excessive adduction only. Placing a knee block more proximally in an attempt to keep the patient back creates pressure against the groin. Instead, you should use strategies to limit forward migration of the pelvis, discussed under posterior pelvic tilt in this previous article on wheelchair pelvic positioning.
What Is the Goal?
It is important to address excessive hip adduction as this could lead to further ROM losses, impacting ADLs such as dressing, toileting, and hygiene.
Hip Abduction
What Is It?
Hip abduction results in the knees moving away from midline.
What Causes It?
Hip abduction may be caused by ROM losses, low tone, or even surgeries. Hip abduction is common in people with Duchenne muscular dystrophy.
How Should I Solve It?
Again, many off-the-shelf cushions include a generic contour to encourage the legs to stay in alignment with the hips. If this is not adequate, lateral knee or thigh supports can be used.
What Is the Goal?
The goals here are to achieve anatomical alignment, if possible, and to prevent pressure of the lateral lower leg against the footrest hangers.

Windswept Posture
What Is It?
A windswept posture is when one leg is adducted and often internally rotated and the other leg is abducted and often externally rotated. As a result, the legs have the appearance of being swept to one side.
What Causes It?
This posture is caused by range limitations, pelvic rotation, and sleep positions. Many patients sleep on their back yet lack full extension of the hips and/or knees. As a result, the legs tend to fall to one side, leading to loss of range and this particular posture.
How Should I Solve It?
The interventions for a windswept posture are the same as those used to address hip adduction and abduction. For example, if the patient is windswept to the right, a medial knee support may be required at the left leg and a lateral knee support at the right.
It may be possible to move the legs into alignment; however, this may pull the patients pelvis into rotation. Ensure the pelvis is neutral and then correct the windswept posture as much as possible while maintaining a neutral pelvis.
What Is the Goal?
The goals for resolving a windswept posture are the same as those for pelvic rotation, as described in the article above:
Supporting the anatomical curvatures of the spine
Promoting weight bearing on the ITs
Achieving alignment for biomechanical function
Providing proximal stability for function
Preventing trunk rotation
Increasing pressure distribution over the posterior trunk
Knee Flexion
What Is It?
The client may position their knees in a flexed position, even past 90 degrees.
What Causes It?
This posture is almost always due to tight hamstrings.
How Can I Solve It?
The hamstrings cross two joints, the hips and the knees. To relieve the pull on the hamstrings, you can either open the seat-to-back angle or decrease the knee angle.
The challenge with decreasing the knee angle, particularly in adults who have longer legs than children, is caster interference. The footplate will hit the front casters and interfere with turns if a 90-degree footrest hanger is used. However, using footrest hangers at 60 degrees may not be possible for someone with tight hamstrings.
Various hanger angles are available, and the footplates themselves can be moved rearward to flex the knee further. Specialty footrest hangers are available to accommodate significant limitations. Many power wheelchairs offer a center-mount footrest hanger to minimize caster interference. Front- and mid-wheel drive power wheelchairs allow 90-degree footrest hangers to be used without caster interference.
What Is the Goal?
The goals for resolving knee flexion include decreasing tension in the hamstrings and the resultant pull into a posterior pelvic tilt. You also want to avoid caster interference and ease transfers.
Knee Extension
What Is It?
The knee is extended beyond 90 degrees of flexion either dynamically or because of loss of range.
What Causes It?
This posture is typically due to increased extensor tone or loss of ROM.
How Should I Solve It?
If this posture is due to increased tone, strategies to reduce tone should be explored. Dynamic options can be very helpful in diffusing force by allowing controlled movement into extension. Strapping the feet to the footplate can limit active extension, if tolerated by the client.
If this is a fixed range limitation, the footrest hanger must match the available range. If this cannot be achieved using standard footrest hangers, elevating leg rests (ELRs) may be required.
What Is the Goal?
The goals here include alleviating the pull on the pelvis and lower leg and accommodating the client in an extended position, as required.
Ankle and Foot Limitations
What Is It?
Any limitation in normal ankle and foot position.
What Causes It?
Limitations of ROM, tonal patterns, lack of weight bearing, and surgery can result in atypical ankle and foot shapes and postures.
How Should I Solve It?
Angle-adjustable footplates (sagittal and frontal planes) are designed to match the angle of the ankle to maximize weight bearing. Standard footplates commonly can accommodate limitations in plantar and dorsiflexion. Specialized footplates can also accommodate limitations in inversion and eversion.
If these footplates cannot adequately distribute pressure, then other strategies are required. Foot boxes, for example, surround the foot to provide protection and support, and adaptive footwear can also distribute pressure and protect the feet.
What Is the Goal?
Goals include protecting the feet from injury, providing comfort, and distributing pressure as much as possible.
What About Carol?
After a thorough assessment, you are able to determine that Carols unusual lower extremity positioning is the result of dynamic hip extension. By opening up her seat-to-back angle, you are able to resolve this uncomfortable and unstable posture, improving Carols comfort and quality of life.
Learn more about assessing and resolving positioning issues of the lower extremities in the Medbridge course, "Wheelchair Seating Assessment: Positioning the Lower Extremities."
Below, watch Michelle Lange discuss hip flexion in wheelchair positioning in a short clip from her MedBridge course, "Wheelchair Seating Assessment: Positioning the Lower Extremities."