Recognizing & Addressing Post-Intensive Care Syndrome (PICS)

“Chuck,” a 54-year-old male, has presented with pain and difficulty walking. He reports that he thinks he has tendinitis, and his past medical history includes diabetes and hypertension, which he has been managing with diet and exercise.
Chuck’s pain began after taking prolonged time off from his exercise routine due to hospitalization for pneumonia, which included five days in the ICU. Fortunately, he did not require mechanical ventilation. Since the hospitalization, however, fatigue, difficulty sleeping and concentrating, and nagging pain in his ankle and foot have prevented him from restarting his exercise routine.
Managing Chuck’s concerns could include rehabilitation services or medication; however, there are indications that other factors are present and impacting his ability to successfully resume his exercise routines. In addition to his potential tendinitis, his fatigue, difficulty returning to exercise, and difficulty concentrating could indicate post-intensive care syndrome (PICS).
What Is PICS?
PICS was first described in 2012 as “New or worsening impairments in physical, cognitive, or mental health status arising after critical illness and persisting beyond acute care hospitalization.”1
Problems associated with PICS fall into these three domains:
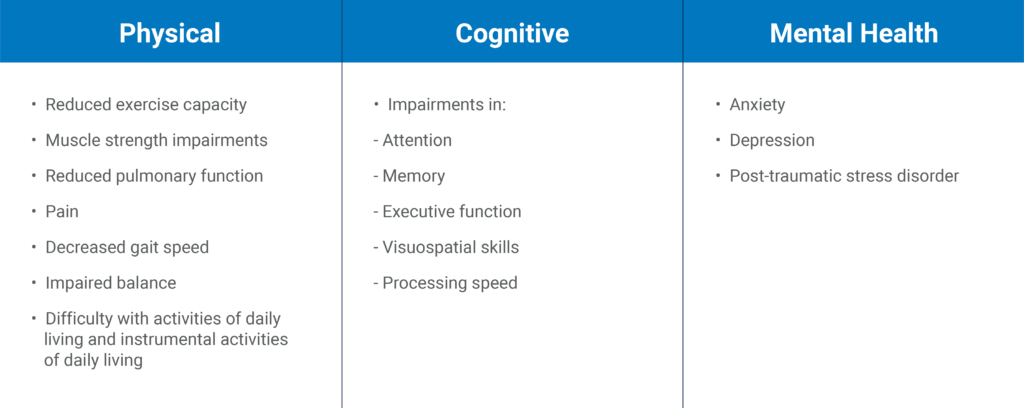
While individual presentations of PICS can vary widely across these domains and in severity, we know that the physical problems associated with PICS are the most common and are present in up to 70 percent of ICU survivors.2
In our MedBridge course, “Recovery from Critical Illness: Recognizing Post-Intensive Care Syndrome,” we review the problems associated with PICS, their prevalence, and risk factors in more detail. We also discuss the impact of critical illness on the families of the ICU survivor, a syndrome known as post-intensive care syndrome-family (PICS-F).
How Is PICS Recognized?
Since PICS is a syndrome, and not a diagnosis of pathology, recognition of PICS depends on the ability of healthcare teams to:
- Readily identify patients who are at risk (i.e. have required care in an ICU)
- Properly screen for the problems associated with PICS
- Engage an interprofessional team for the management of the individual patient’s needs
The interprofessional team may include:
- Rehabilitation professionals such as physical therapists, occupational therapists, and speech-language pathologists
- Registered nurses and physicians, including primary care and specialists such as pulmonologists
- Mental health professionals such as social workers, psychologists, and psychiatrists
Are There Recommended Tests and Measures for PICS?
Yes!
In our course, “Recovery from Critical Illness: Examination and Evaluation for PICS,” we review specific examination and outcome measures for the physical problems associated with PICS, as well as screening tools for the cognitive and mental health problems associated with PICS, such as the Montreal Cognitive Assessment and the Impact of Events Scale–Revised (IES-R).
Using these tools regularly can aide in developing a prognosis and plan of care as well as guide referrals within an interprofessional team to ensure optimal outcomes for survivors of critical illness.
What About Interventions for PICS?
Multiple interventions can improve the physical problems associated with PICS —when these interventions are designed and dosed properly. Selecting interventions and using them judiciously is the focus of the third course in our series, “Recovery from Critical Illness: Physical Rehabilitation for PICS.”
Interventions we recommend include:
- Patient and family education
- Energy conservation strategies for prioritizing activity and participation in the presence of fatigue or reduced stamina
- Compensatory strategies, such as repetition of messages and paraphrasing to ensure comprehension
- Restorative exercise relevant to the patient’s goals and current limitations
- Strategies to promote participation within the community
- Pain relief
- Coping strategies for prolonged recovery
Intervention goals may change based on the acuity and severity of the person’s impairments and activity limitations, all of which are discussed in detail in this course.
Proper identification of people who are experiencing PICS in post-acute, outpatient, and home health settings is important for their recovery. Following PICS identification with directed treatments and/or referrals is key to promoting optimal outcomes and return to meaningful life roles.
Take the time to learn more about PICS and join us for one or all of the courses in this series.
- Needham, D. M., Davidson, J., Cohen, H., Hopkins, R. O., Weinert, C., Wunsch, H., & Zawistowski, C., et al. (2012). Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Critical Care Medicine, 40(2), 502–9.
- Van der Schaaf, M., Beelen, A., Dongelmans, D. A., Vroom, M. B., & Nollet, F. (2009). Poor functional recovery after a critical illness: a longitudinal study. Journal of Rehabilitation Medicine, 41(13), 1041–8.