Getting Started with Standardized Care Pathways: A Primer for Hospitals and Health Systems

As hospitals and health systems transition away from the traditional fee-for-service model and begin to adopt value-based care and bundled payments, many healthcare leaders are looking towards standardized care pathways as a way to improve quality of care while reducing costs.
With that in mind, this article provides an overview of standardized care pathways, including why hospitals and health systems typically adopt them, how to structure an effective care pathway, what benefits to expect, and how to measure results.
Why now: Common drivers for adoption
The three most common reasons organizations adopt standardized care pathways are to improve quality of care, reduce costs, and boost patient outcomes. More specifically this might look like a need to:
- Improve patient outcomes for complex patients, chronic conditions, and bundled programs such as total joint replacement (TJR), neurological disorders, spine problems, congestive heart failure, and stroke.
- Create effective, standardized pre-op and post-op programs that reduce costs by improving operational efficiency and quality of care. Standardizing these programs alone can result in significant savings; for example, up to $1,500 per hip and knee replacement.1
- Help patients learn how to better self-manage their conditions and be active partners in their care.
Ensure that clinicians are following consistent, standardized clinical practice guidelines.
Benefits of care pathways
Successful care pathways typically include best practices based on clinical evidence for treating and educating patients, and training clinicians and caregivers. This results in:
- Improved patient understanding, self-management, and buy-in.
- Better patient engagement, adherence, and outcomes.
- Improved staff competency and efficiency.
- The ability to provide the right level of care at the right time through a mix of in-person and virtual visits.
- Effective monitoring of patient adherence in order to remediate gaps.
Common challenges to implementing a care pathway
If your organization is considering developing and implementing care pathways, it’s good to be aware of some of the difficulties you might encounter so that you can plan ahead to mitigate them. Three of the most common challenges include:
- Successfully collaborating across departments to develop a more integrated approach to patient care.
- Navigating change management within teams.
- Achieving buy-in from providers.
Anatomy of a successful care pathway
Standardized care pathways help organizations more effectively manage a wide spectrum of common conditions and improve outcomes by planning out the steps in a patient’s journey throughout an episode of care, from intake through rehabilitation, for their particular condition.
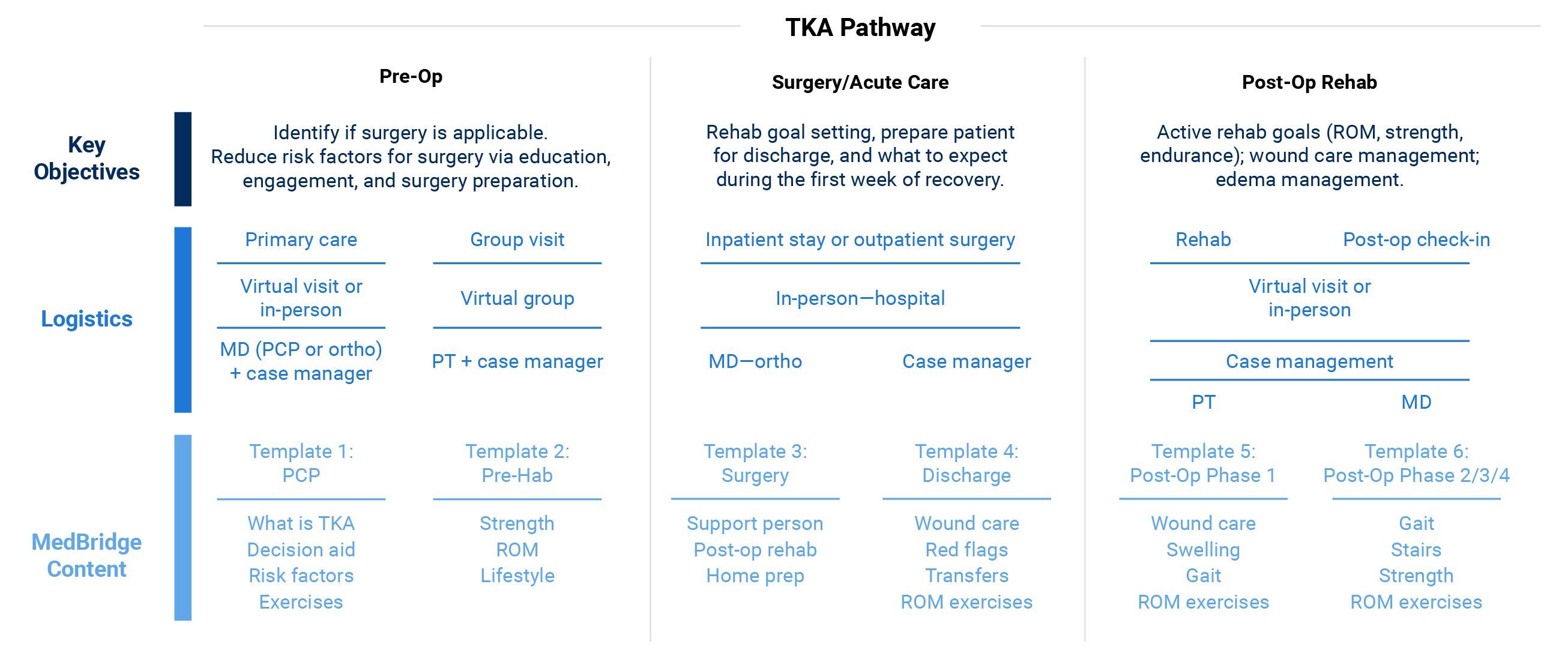
An effective care pathway maps out four main categories—key objectives, logistics, patient programs, and outcome measures—for each stage of the patient journey.
Key objectives are the primary goals for patient treatment and recovery at each stage, such as educating the patient on what to expect, reducing risk factors, and achieving rehab benchmarks.
Logistics address what type of care is delivered, and by whom, during each stage of the patient journey; for example, virtual care delivered by a physical therapist or in-person care delivered in the hospital.
Patient programs detail the patient education and engagement tools, such as home exercises, that will be used during the plan of care to help inform patients about their condition, encourage adherence, reduce risk factors, and set them up for success.
Outcome measures are the quality benchmarks your organization aims to achieve. They help you identify patients who are off track, make targeted improvements, and support all patients to achieve discharge and recovery goals.
Level up your care pathway with a training plan for your team. It’s likely that you’ll see even better results if you include targeted, condition-specific clinical education and best-practice training to improve clinician expertise, boost interpersonal skills, and help clinicians provide high-quality virtual care.
Here’s an example of a care pathway for total knee arthroplasty (TKA) used by one health system:
How is the success of a care pathway measured?
After implementing a care pathway, it’s important for an organization to be able to monitor progress, measure success, and make improvements as necessary. Three key benchmarks to monitor are:
Cost per episode
Current research indicates that a shift towards value-based care significantly reduces costs. Is this the case for your care pathway? How much does it cost to manage a patient from intake or pre-op through to outpatient? Have margins and reimbursements increased?
Outcomes
Are patients achieving optimal outcomes within the care pathway as measured by function, readmissions, and post-op complication? Have your quality measures improved and referrals increased?
Patient engagement and satisfaction
Are patients engaged and following through with their program, and are they satisfied? If not, take a look at whether patients are receiving programs pertinent to their condition in a timely manner and if they are consistently accessing them. High patient adherence and satisfaction are important for improving outcomes, increasing member retention, and helping to boost plan ratings.
How MedBridge can help
MedBridge offers an integrated solution that allows organizations to build highly successful pathways of care. To see how this works in action step by step, view our infographic.