Ditch the Treatment Table: How to Assess and Treat with Reference and Relative Motion

A significant portion of rehabilitation consists of movement. Observational gait assessment, functional movement assessment, body mechanics training, and return-to-sport training are just a few of the things rehab professionals and athletic trainers do that require knowledge of movement. However, not all movement is the same.
Movement can be categorized using the following groups:
- Open kinetic chain versus closed kinetic chain
- Single-joint versus multi-joint
- Slow/static versus fast/dynamic
- Reference versus relative
Here, we will explore the roles of reference motion versus relative motion in assessing and treating athletes of different sports.
What Are Reference Motion and Relative Motion?
Reference motion is a movement that occurs at the body region of interest. Relative motion is a movement that occurs at an area adjacent to or near the body region of interest due to the initiation of reference motion. These definitions are a bit abstract and may make more sense with an example.
Starting from an anatomical position, if you raise your right leg out to the side, you have just abducted one hip joint (fig. A). This movement is an example of reference motion; the hip is our reference. Now imagine starting from an anatomical position where you shift your pelvis to the left (fig. B). The reference motion in this example was the pelvis performing left translation; however, the right hip should also now be relatively abducted! That is the relative motion.
Try to think of other examples of relative motion. The simplest kinds are usually in a closed kinetic chain where a proximal body segment is initiating movement, which then causes the distal segments to undergo relative motion.


What Is the Importance of Distinguishing Between Reference and Relative Motion?
We make these distinctions because of the complexity of human movement. In function, during any given action, there are often many other joints or body areas undergoing relative motion. People do not move one joint at a time in isolation.
Think about how many joints and body regions must move and interact when reaching up into a cabinet for a cup. From finger extension to shoulder flexion to thoracic rotation, each movement plays an integral role. When assessing and treating a patient or athlete, the type of movement is a critical factor for the therapist to individualize the care they provide.
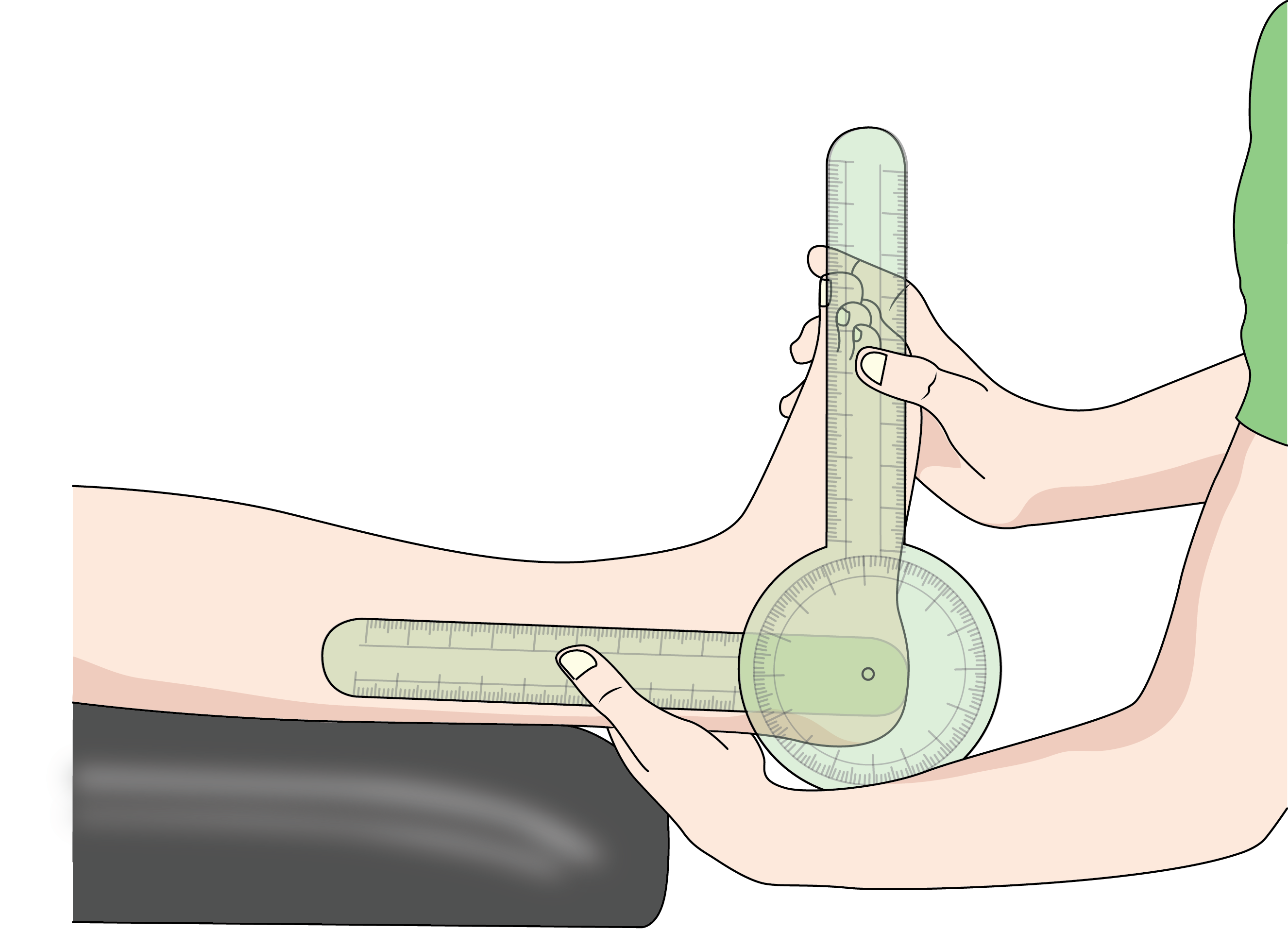
For example, consider the case of rehabilitating a basketball player after an ankle sprain. Dorsiflexion range of motion performed with a goniometer in supine may help track progress (fig. C); however, this movement is unlikely to occur during basketball play. It would be more appropriate to assess dorsiflexion in standing during a squat or knee-to-wall assessment (fig. D) because this more closely replicates the conditions in which the player will be using this range of motion in function (fig. E).


Assessment and Treatment: Reference vs. Relative
Now let’s look at treating the same problem in two different athletes. Painful, limited hip internal rotation range of motion (ROM). The first example will employ reference motion; the second will employ relative motion.
Example of Reference Motion—The Swimmer
Imagine you are seeing an athlete in the clinic for their initial evaluation. The athlete is a competitive swimmer who has right hip pain during the breaststroke portion of their individual medley. Specifically, the pain occurs during the whip kick of their breaststroke, which is the last and most powerful movement during the stroke.
During this movement, the hip must flex and internally rotate then extend quickly. Knowing this, you will assess the patient in a seated position to determine their active and passive hip internal rotation ROM in 45 degrees of hip flexion (fig. F). Hip internal rotation is our reference motion in this case. Determining it is limited, with a capsular end-feel compared to the asymptomatic side; this restriction is the clear cause of the symptoms.
his discovery can warrant a lateral distraction mobilization with movement of the right hip or a contract relax technique, prepositioned in internal rotation to improve the patient’s active and passive ROM (fig. G) which makes the most sense in this situation because both in the mobilization and during the breaststroke (1) the patient’s pelvis is relatively stable, (2) the patient’s hip is actively contracting in open kinetic chain, and (3) the patient’s hip is positioned in internal rotation.


From here, any internal rotation exercise can be applied to follow up the manual intervention and improve the patient’s ability to utilize their new ROM. However, the most applicable intervention will directly mimic the mechanics during swimming, just like the joint mobilization treatment did.
For example: Position the patient on their knees with forearms on a Swiss ball. Then, with their hips flexed to about 45 degrees and their knees flexed so that their feet are in the air, the patient would internally rotate one or both hips actively. Resistance can be added as you see fit. The specific method in which this exercise is completed mimics many of the same conditions as swimming itself:
- The patient is in a prone position.
- The Swiss ball creates some rotation instability, similar to water.
- The patient is in 45 degrees hip flexion, as well as in the whip kick.
- The movement is hip-on-pelvis, as it is during the whip kick (hip internal rotation is our reference motion).
Next, we will cover the relative motion example for the same impairment in a tennis athlete. As you read along, try to compare and contrast similarities and differences.
Example of Relative Motion—The Tennis Player
Your patient is a competitive tennis player who experiences right hip pain during and after games. The right leg is their lead, and the pain is greatest during the follow-through of their forehand swing. You find a lack of internal rotation ROM in the right hip. You could test from a seated position as in the previous example of the swimmer; however with the demands of the tennis forehand, the hip is not flexed much at all, and the measurement would be best taken in a more neutral hip position. Furthermore, when the player performs a forehand, the right foot is planted and stable against the ground.
The reference movement for this patient is right trunk/pelvic rotation, which is causing the relative internal rotation of the right hip; thus, it is more appropriate to measure relative hip internal rotation (IR) in closed kinetic chain, standing, with their pelvis initiating the movement.
For example, the patient can stand on an excursion mat or set of three intersecting pieces of tape that create an asterisk pattern. The patient will place their right heel on the center of the tape and then step their left foot around to rotate their right hip relatively internally. If you imagine a line going from one ASIS to the other, you could compare the line from the patient’s starting position to their end position to read the angle of internal rotation.
Much like in the example of the swimmer, treatment for this impairment will have less to do with the actual demands of tennis and more to do with increasing the patient’s internal rotation and improving their ability to utilize their ROM.
Use your hands to pre-position the right thigh in internal rotation and then instruct the patient to perform the same movements as the assessment above. This creates a greater stretching effect. This treatment could be enhanced with a Theraband wrapped around the thigh to create further internal rotation force. Further progression includes a resistance band wrapped around the pelvis pulling posteriorly on the left side, which would resist the patient’s movement into right pelvic rotation, or relative internal rotation.
Ongoing Implementation of Reference and Relative Motion
As you further uncover the differences between reference motion and relative motion, you’ll find more useful ideas for assessment and treatment strategy to help individualize the care for each patient and differing types of athletes.
Here are a few key takeaways to remember when trying to devise ways of assessing and treating movement in patients:
Does the assessment/treatment:
1. Mimic the kinetic chain conditions of the functional activity (OKC/CKC)?
2. Mimic the general body position of the functional activity (prone/supine/flexed/extended)?
3. Mimic the muscle action of the functional activity (concentric/eccentric/isometric)?
4. Mimic the relative or reference motion conditions (where is the movement initiated)?
5. Mimic the body-on-limb or limb-on-body conditions?
Now that you have the basics of relative motion and functional assessment, you can adapt these strategies to any sport or movement. For further guidance on how to treat patients with more specificity, efficiency, and ease, I offer a variety of MedBridge courses tailored to varying forms of movement and plans of treatment.

