5 Solutions for a Better Fall Prevention Program
April 14, 2023
5 min. read

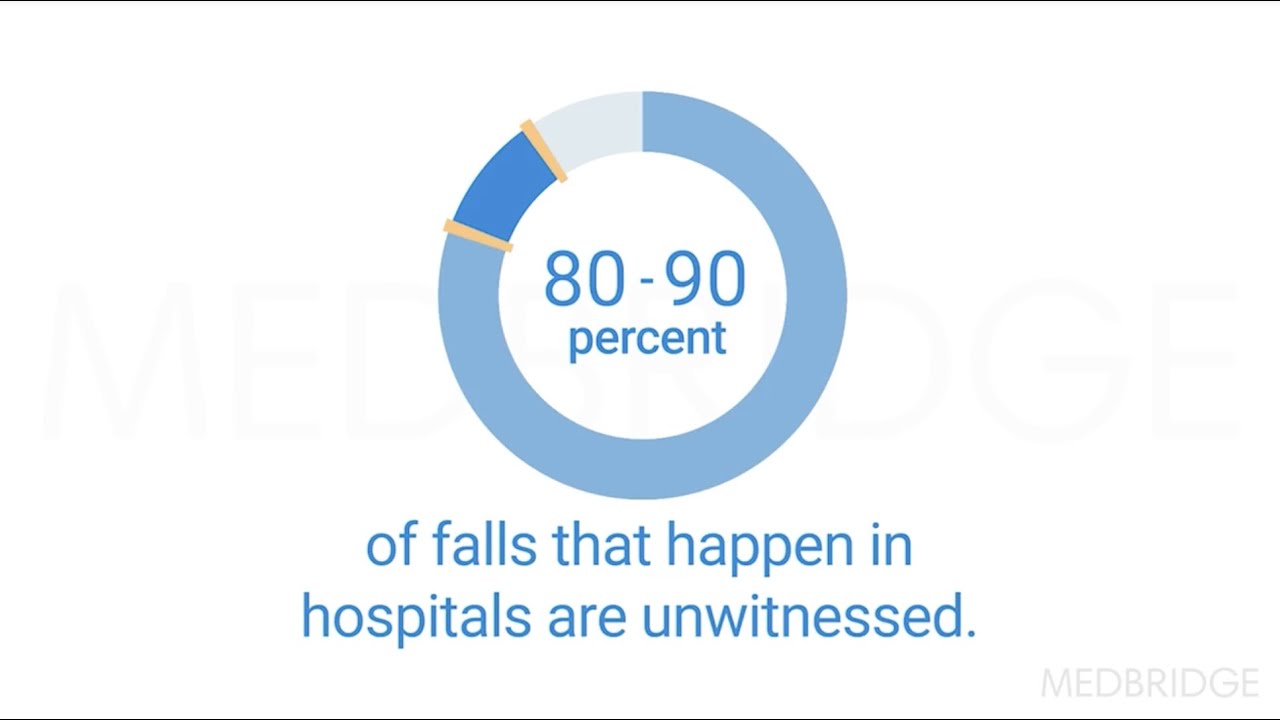
Across all settings, patients are still falling in our care, and some are experiencing recurrent falls. Even patients admitted due to a fall are falling in our care! Despite decades of research and resources invested in patient safety, falls continue to be the most reported patient safety incident in hospitals.1 Falls are considered a never event, yet they remain a common and devastating complication of hospital and post-acute care, particularly in geriatric patients.2
We must do better to protect our patients from preventable falls and resulting injuries. As registered nurses and rehabilitation specialists, we know the compassionate, diligent, and competent care required to keep patients safe. By providing and validating clinicians' essential knowledge specific to fall prevention management, patient education and engagement, and post-fall management, we can assure a minimum knowledge base for all clinicians at the point of care.
The Problem with a Universal Approach to Fall Prevention
For years and across bodies of research, including comparative studies without randomization, cohort studies, and case-control studies, the primary outcome measure to determine the effectiveness of fall prevention programs has been the fall rate. The secondary outcome has been and continues to be the fall injury rate.3
In many units, the measure of fall prevention program success posted to the public, displayed in nursing conference rooms or unit hallways, are run charts of aggregated fall and fall injury rates over time. These data fail to inform program effectiveness. Rather, success should be reported as improvement in patients' health, function, and independence, achieved through individualized fall prevention care management by specialty-prepared clinicians.
An aggregated outcome measure does not provide evidence of the effectiveness of program structures and processes. Unfortunately, most organizations are not measuring the efficacy of the individual components of their clinical fall prevention education programs:
Fall risk assessment structures and processes, such as identification of each patient fall and injury risk factors, both modifiable and non-modifiable
Fall prevention care delivery, including individualized care planning, implementation, and evaluation of patients' response to care
Patient education programs to build patient knowledge and skill
Post-fall management programs on mitigating and eliminating root causes of falls and harm
Fall & Injury Prevention PDF
Fill out the form to unlock your free Fall Prevention assessment!
Unlock Resource
A Different Approach to Fall Prevention Programs
Fall prevention programs are complex and must factor in the dynamic influences of organization and unit structures and processes, the ever-changing risk factors of each patient, and the varying levels of clinicians knowledge, experience, and competencies. Preparing a workforce that provides competent, skill-based care that meets national standards requires an expert-prepared, competency-based program.
Lets explore five evidence-based organizational solutions for better fall prevention:
Solution 1: Focus on fall and injury risk assessment over fall risk score.
All patients require a risk screen, which prompts an in-depth assessment upon admission. The complexity of fall risks requires comprehensive interdisciplinary assessment, care planning,4 and the integration of interactive patient-to-nurse communication technology.
This in-depth assessment should trigger an interdisciplinary care team approach to seek, treat, mitigate, and/or eliminate the underlying cause of the identified risk factors that contribute to preventable falls, resulting injuries, loss of function, and possibly, life.
Solution 2: Engage patients as full partners in their fall prevention program.
Clinicians lack the in-depth knowledge and skills to evaluate the effectiveness of their teaching and their patients cognitive knowledge and psychomotor skills. Evidence confirms that patient outcomes improve when patients and caregivers are fully engaged as partners in their care.5 Interventions that tailor patient education to each patients level of engagement as a partner in their fall prevention program build the skills and confidence to prevent and manage falls.
Solution 3: Stop unsafe toileting and start individualized toileting programs.
Many hospital-based fall-prevention programs include toileting rounds, without evidence of effectiveness. The range of toileting-related falls in bathrooms was reported to be 38 percent to 47 percent.6
Many organizations are mandating that no patient toilets alone, or that nurses stay within arms reach. These programs have limited evidence of effectiveness, are not feasible with existing staffing, and violate patient autonomy and privacy. Importantly, alternatives for technology integration are needed to meet patient and nursing staff needs.
Solution 4: Take actions to intentionally eliminate root causes of falls and injury.
Post-fall huddles (PFH) with nurses and interdisciplinary staff are essential after a fall has occurred. Unfortunately, many clinicians do not possess the necessary management skills to determine root causes of falls and injury, implement strategies to mitigate and eliminate these root causes, and prevent repeat falls based on the same root causes.
These skills are critical to improving patient safety. PFHs and assessments must be conducted in all settings of care to determine the cause of the fall, and intervene appropriately.7,8
Solution 5. Analyze fall prevention programs based on precision and rigor rather than an aggregated fall rate.
Analysis of fall prevention programs requires more than an examination of aggregated fall rates. Program evaluation is the process of evaluating structures and processes that lead to improvements in outcomes. The results of these evaluations should inform rehabilitation, including all nurses and teams, about the structure and process of fall and fall injury program attributes at the organization, unit, and patient levels.
This level of program assessment leads to opportunities to enhance practice, clinical skills, and program infrastructure and capacity. As a result, all nurses are better positioned as clinical leaders to implement and spread interventions to improve patient and program outcomes.
My five-course Medbridge certificate series will inspire you to implement change in your fall prevention program. You'll go beyond an over-reliance on fall risk screening and universal fall precautions and feel competent in implementing a more comprehensive fall prevention program that incorporates the five solutions discussed above and much more. Medbridge boasts a rich portfolio of fall prevention courses that span topics such as patient education/engagement, discharge planning, care coordination, and caregiver support.
Below, watch Pat Quigley discuss the post-fall huddle in this short clip from her MedBridge course, "Post-Fall Management for Rehabilitation Nurses."